Podcast: Play in new window
Subscribe: RSS
Date: April 12, 2023
Reference: Weizmann et al. Incidence of Cardiac Arrest During Sports Among Women in the European Union. JACC November 2022
Guest Skeptic: Dr. Susanne (Susy) DeMeester is an Emergency Physician practicing at St Charles Medical Center in Bend, Oregon. She has been very involved with EMRAP’s CorePendium as the cardiovascular section editor.
Last time Susy was on the SGEM it was for an SGEM Xtra episode discussing gender issues related to cardiovascular disease. Here are five of the highlights from that episode:
 The leading cause for morbidity and mortality in both males and females is cardiovascular disease (CVD)
The leading cause for morbidity and mortality in both males and females is cardiovascular disease (CVD)- Females are often excluded from being subjects in medical research, included CVD research
- Most male and female patients with myocardial infarctions still present with chest pain. However, women are more likely to have atypical presentations compared to men (shortness of breath, weakness, and fatigue).
- In addition to the usual cardiac risk factors, females also have other things that increase risk like pregnancy, hormone replacement therapy and autoimmune diseases
- Females diagnosed with acute coronary syndrome are less likely to receive timely therapies
Case: You are reading through your social media feed and see a story that jumps out at you. It is a report of a seemingly invincible athlete who collapses on the field and dies of sudden cardiac death. It reminds you of the recent case of football player Damar Hamlin, who has thankfully recovered well. This story makes you wonder: when was the last time you heard of a sudden cardiac death in the female athlete?
Background: Sudden cardiac arrest (SCA) is a rare but serious event that can occur in athletes during training or competition. While it can occur in both male and female athletes, the incidence is reported to be higher in male athletes.
There are several reasons why SCA may be more common in male athletes than in female athletes. One reason is that male athletes tend to participate in sports that involve more physical contact and higher levels of exertion, which can put more strain on the heart. Additionally, male athletes are more likely to have certain genetic predispositions to heart conditions that can increase their risk of SCA.
However, it is important to note that SCA can occur in female athletes as well, and it should not be ignored or overlooked. Females who participate in high-intensity sports should undergo appropriate cardiovascular screening to identify any underlying heart conditions that could increase their risk of SCA.

Females are increasingly competing in recreational and professional sports. Little seems to be heard about SCA in these athletes. In fact, not surprisingly, there is a paucity of data on the subject. However, currently available evidence suggests we can improve our understanding of SCA in all athletes by examining sex-based differences.
Clinical Question: What are the sex-based differences in sports related SCA?
Reference: Weizmann et al. Incidence of Cardiac Arrest During Sports Among Women in the European Union. JACC November 2022
- Population: Three large European registries that prospectively collect data on every case of SCA between 2006-2017. Sports-related (Sr) SCA was defined as occurring <=1 hour after ending a sports activity.
- Excluded: Patients not referred to registry and patients with SCA greater than one hour after cessation of sport.
- Intervention: There was no intervention as this was a prospective data analysis
- Comparison: Sr-SCA in men vs women
- Outcome: Incidence, characteristics, and outcomes in women vs men after episode of Sr-SCA
- Type of Study: Prospective observational registry study
Authors’ Conclusions: “These findings emphasize the dramatically lower risk of Sr-SCA in women compared with men, despite similar subject characteristics. This should be considered in designing preparticipation screening strategies in the future.”
 Quality Checklist for Observational Study:
Quality Checklist for Observational Study:
- Did the study address a clearly focused issue? Yes
- Did the authors use an appropriate method to answer their question? Yes
- Was the cohort recruited in an acceptable way? Yes
- Was the exposure accurately measured to minimize bias? Yes
- Was the outcome accurately measured to minimize bias? Unsure
- Have the authors identified all-important confounding factors? Unsure
- Was the follow up of subjects complete enough? Yes
- How precise are the results? Fairly precise
- Do you believe the results? Yes
- Can the results be applied to the local population? Unsure
- Do the results of this study fit with other available evidence? Yes
- Funding of the Study: Funded by variety of scientific grants. There was also grant money from companies ie, Boston scientific, Medtronic, and Zoll, though authors did not have any relationships to disclose.
Results: They were 34,826 cases of SCD between 2006-2017 in the three registries. A total of 760 (2.2%) were classified at as Sr-SCD. Of those cases, 54 women (7.1%) and 706 men (92.9%).
Key Results: Sports-related SCA was much more common in men than women
- Primary Outcome: Incidence of Sr-SCA was 0.19 per million women per year vs 2.63 per million men per year
Management and survival at hospital admission were similar. Patients received bystander CPR at similar rates and similar time frame. Survival to admission was 58% in both men and women. Patients also had similar 30 day and 1 year survival.
 1. Registry Data: Even though the data was collected prospectively, it is still an observational study. There could be unmeasured confounders biasing the data. We have already mentioned that patients who were deceased prior to EMS arrival is problematic. It introduces selection bias into the data set. There were also very few events (54 Sr-SCA) in women, and we need to be cautious about making any conclusions with such limited data.
1. Registry Data: Even though the data was collected prospectively, it is still an observational study. There could be unmeasured confounders biasing the data. We have already mentioned that patients who were deceased prior to EMS arrival is problematic. It introduces selection bias into the data set. There were also very few events (54 Sr-SCA) in women, and we need to be cautious about making any conclusions with such limited data.
2. Baseline Demographics: We do not know much about these women. They authors provide in Table 2 age, history of heart disease and whether the women had at least one cardiovascular risk factor. These included known/treated diabetes mellitus, dyslipidemia, systemic hypertension, obesity, any smoking. However, we know there are other women specific risk factors such as pregnancy, hormone replacement therapy, and autoimmune disease.
3. External Validity: These were three registries of mainly white European women from Paris, Amsterdam, and Sweden mainly in urban environments. Whether this applies to non-white, non-European, rural women is unclear.
4. Details of Activity: The registries did not have the most comprehensive data about type of activity and intensity and background frequency the activity was being performed. Also did not know if it was recreational or competitive sports being performed at the time of the SCA.
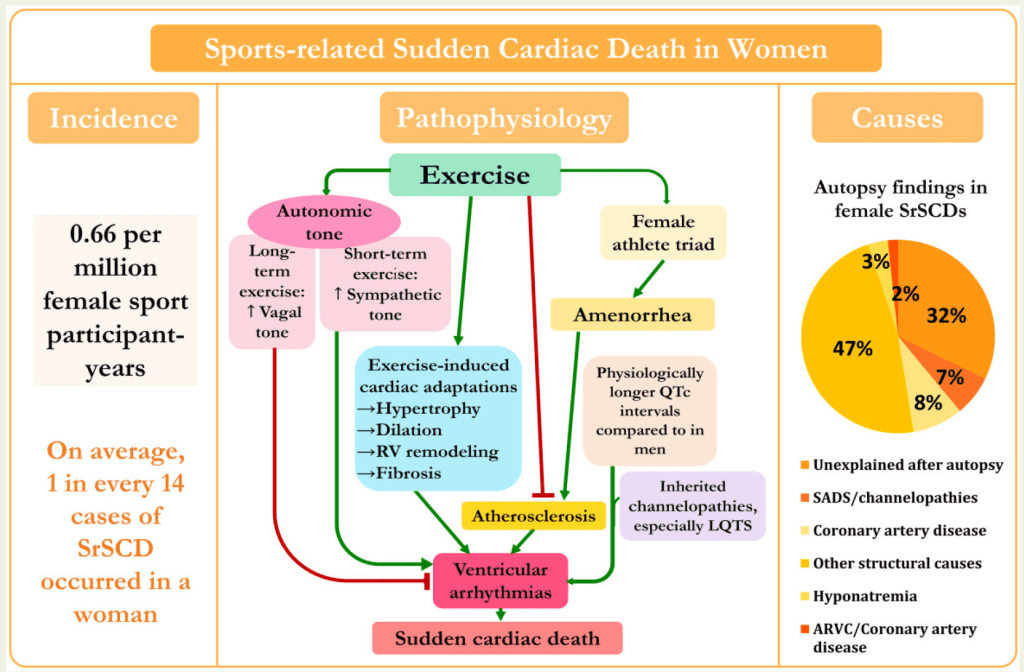
5. Why the Difference: The authors did not go into much exploring why there was such a huge difference in Sr-SCA between men and women. They talked about ACS being less common in women, estrogen, and higher vagal tone being protective. However, there is a great review article from the European Society of Cardiology on Sr-related SCA by Rajan et al. It did a nice job of jumping into the ‘why’ reasons for the differences between men and women. It was published in 2022 and included an epidemiology review, with findings similar to the JACC study we have been discussing. It was particularly good that they reported findings as females per million female sport participants. They then explored the physiologic adaptations to exercise that distinguish women from men.
- Changes in the Left Ventricle:
- Left ventricular wall thickness (LVWT) and left ventricular hypertrophy (LVH) greater was in male athletes of similar age and training intensity. Proposed etiology is related to of effects increased angiotensin and testosterone in men. LVWT and LVH are associated with increased ventricular arrhythmias.
- If you see ECG findings concerning for LVH in female athlete (especially with lateral t-wave inversion, ST changes) you should be worried.
- Right ventricular remodeling and arrhythmogenic right ventricular cardiomyopathy (ARVC) is much more common in men.
- Myocardial fibrosis because of exercise also more common in men (MRIs of athletes showed 17% in men and none in women). Likely related to lower blood pressure and estrogen effects. Fibrosis is another impetus for dysrhythmias
- Coronary Artery Disease (CAD) is overall the most common cause of SCA, including in Sr-SCA. However, CAD as etiology much less common in women. Men more likely to suffer plaque rupture/thrombosis, women at risk for microemboli and microdysfunction, but these are better tolerated and less likely to cause Sr-SCA.
- Spontaneous Coronary Artery Dissection (SCAD) is a tear in an artery wall in your heart that allows blood to build up in the space between the layers of your artery wall.It is commonly associated with the middle-aged women. However, in the setting of Sr-SCA, is surprisingly more common in men.
- Takostubo is much more common in women, to review global LV dysfunction brought about by emotional or physical stress [catechol excess] and can lead to SCA.
- Structural heart disease is much more common in men as an etiology. Women more likely to have no underlying structural abnormalities. In this ESC report, 42% of Sr-SCA are not structural vs 4% in men. Most common reasons for Sr-SCA in women are long QTs (LQTs), channelopathy, malignant accessory pathway Therefore, screening echo would likely have a lower yield for women.
- Autonomic tone is much lower in women, making them less prone to catechol surges and arrhythmia.
- QT interval- women more at risk for SCA and Sr-SCA. Have a higher rate of LQTs, are more susceptible to combination of contributing factors. The authors explain it as a ‘mulit hit model’– combo of offending medications, sports, especially in first half of the menstrual cycle (who knew). Diagnostic pearl here, female athletes with QT over 480 ms need more work up and education (ie let them know, specifically in regards to medications to avoid)
- Steroids predispose to Sr-SCA and are much more commonly used in men.
Conclusions from ESC on the topic of sports-related sudden cardiac arrest:
- Coronary artery disease is an unlikely cause in women
- Structural heart disease is unlikely cause in women
- The most common issues are channelopathies, LQTs, and accessory pathways
Comment on Authors’ Conclusion Compared to SGEM Conclusion: The authors’ conclusion was that Sr-SCA is indeed much less common in women. We should consider this when developing public health screening programs.
This is where some additional reading led us to modify the conclusion. While Sr-SCA death is uncommon in women, it is important to understand the underlying etiologies as this should lead to different considerations in screening. Again, unlike men, structural abnormalities and ACS are unlikely etiologies, with SCA related to sudden dysrhythmias death due to channelopathies, long QT, things like ECG, history, and family history are more critical than echo and PCI.
SGEM Bottom Line: Sr-SCA is less common in women and more likely related to dysrhythmia than structural abnormalities and CAD.
Case Resolution: N/A

Dr. Susanne DeMeester
Clinical Application: Differences in underlying mechanisms responsible for Sr-SCA in both men and women can be used to improved public health policy, in particular screening of athletes. And as evidenced from recent newsworthy events, timely bystander CPR and automated external defibrillator application works.
What Do I Tell a Patient? If seeing a patients with sports related syncope or near syncope, I would let them know I am concerned, look closely and their ECG and ask specific questions about their family history. Then I would tell them I am referring them to a cardiologist.
Keener Kontest: There was no question last week and therefore no winner. Listen to the podcast for this weeks’ keener question. If you think you know the answer then send an email to thesgem@gmail.com with “keener” in the subject line. The first correct answer will receive a cool skeptical prize.








You must be logged in to post a comment.