Podcast: Play in new window
Subscribe: RSS
Date: January 4th, 2023
Reference: Hasbrouck et al. Acute management of atrial fibrillation in congestive heart failure with reduced ejection fraction in the emergency department. AJEM 2022
Guest Skeptics: Dr. Timlin Glaser currently a fourth-year resident in emergency medicine at Lehigh Valley Health Network and future medical toxicology fellow at the University of Arizona College of Medicine – Phoenix.
Dr. Matt Murphy is currently a third-year resident in emergency medicine at Lehigh Valley Health Network. He has interests in FOAMEd and is currently following the EBM track in his residency. Welcome to the SGEM Matt.
This episode is recorded live as an SGEM journal club. There are five rules to journal club
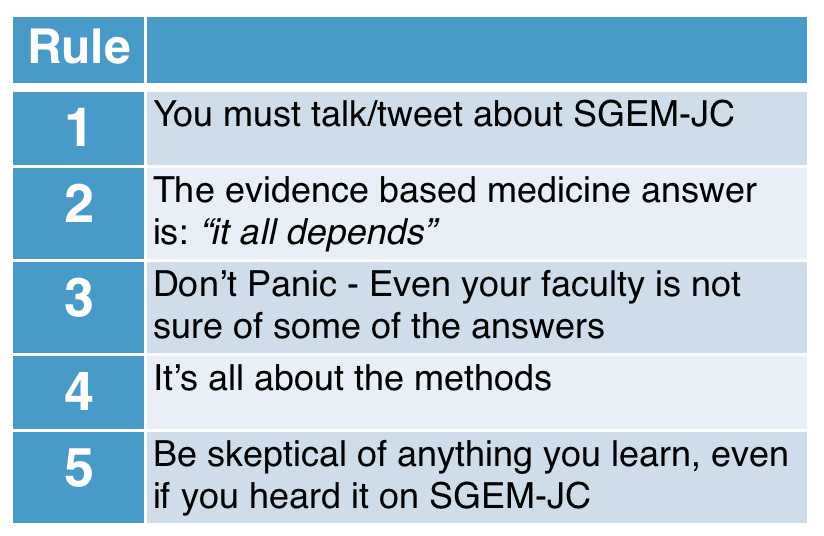
1) You Must Talk/Tweet about SGEM-JC: The SGEM is a knowledge translation project. We know that it can take over ten years for high-quality, clinically relevant information to reach the patient. As Sir Mark Walport famously said: “science is not finished until it’s communicated.”

2) The EBM Answer Is “It All Depends”: This rule was learned this from my EBM mentor Dr. Andrew Worster. There are lots of nuances to the application of the literature. It requires critical appraisal skills, clinical judgment and asking the patient about their values and preferences.

3) Don’t Panic – Even Your Faculty Is Not Sure of Some of the Answers: It is hard to stay up on all the relevant medical literature. There is a tsunami of new information being published every day. It can be overwhelming at times. Don’t panic. As Professor Feynman said…It’s ok to say: “I don’t know”.

4) It’s All About the Methods: The method section is the most important section of the paper. We just said there is so much research being published every day. It can be like drinking from a fire hose making it difficult to find the signal in all the noise. As Professor Altman said in the BMJ back in 1994; “we need less research, better research and research done for the right reasons.” This means we need to be asking the right questions that have patient-oriented outcomes and use proper high-quality methods to answer those questions.

5) Be Skeptical of Anything you Learn, Even If You Heard It On the SGEM Journal Club: Skepticism is such an important concept to understand the medical literature and navigate through life. Aristotle advocated for this thousands of years ago and encouraged people to “be a free thinker and don’t accept everything you hear as truth. Be critical and evaluate what you believe in.”

Case: A 62-year-old male with a past medical history of heart failure with reduced ejection fraction presents to your emergency department (ED) via ambulance for palpitations and shortness of breath that started earlier that day. He arrives with an irregular heart rate of 142 beats per minute (bpm). The remainder of his vital signs are unremarkable. On physical exam, you notice three plus pitting edema of both lower extremities and bibasilar rales when auscultating his lungs. He takes multiple medications at home, including a beta-blocker, an angiotensin converting enzyme inhibitor (ACEi), and a loop diuretic. You order an ECG and confirm the patient has atrial fibrillation (AF) with rapid ventricular response (RVR). The patient is very symptomatic, and you need to decide which pharmacologic agent you will use to treat his current condition.
Background: Atrial fibrillation is a common dysrhythmia seen on a regular basis by emergency physicians. We have covered this topic several times on the SGEM including:
- SGEM#88: Shock Through the Heart (Ottawa Aggressive Atrial Fibrillation Protocol)
- SGEM#133: Just Beat It (Atrial Fibrillation) with Diltiazem or Metoprolol?
- SGEM#222: Rhythm is Gonna Get You – Into an Atrial Fibrillation Pathway
- SGEM#260: Quit Playing Games with My Heart – Early or Delayed Cardioversion for Recent Onset Atrial Fibrillation?
- SGEM#267: AFib of the Night – Chemical vs. Electrical First Cardioversion

As discussed in SGEM#133, clinicians routinely employ beta blockers or calcium channel blockers (CCBs) for rate control in patients with AF. Multiple studies have demonstrated that both agents are effective in decreasing ventricular rate to an acceptable range, and current AHA guidelines approve their use in uncomplicated AF.
However, the use of beta blockers and non-dihydropyridine calcium channel blockers for rate control in patients with AF with RVR and concurrent decompensated heart failure with reduced ejection fraction (HFrEF) remains controversial.
Current guidelines specifically recommend against the use of CCBs (1) despite limited evidence (Level C). For the ED clinician, such a scenario poses a conundrum, as both the disease process and the intervention can worsen heart failure and contribute to cardiogenic shock.
Clinical Question: In patients with HFrEF presenting to the ED in AF with RVR, are there significant differences in adverse outcomes for patients treated with IV diltiazem vs IV metoprolol?
Reference: Hasbrouck et al. Acute management of atrial fibrillation in congestive heart failure with reduced ejection fraction in the emergency department. AJEM 2022
- Population: Adult patients 18 years of age or older who presented to the ED with Atrial Fibrillation with Rapid Ventricular Response and had a formal echo with an EF less than or equal to 40% during the same encounter
- Excluded: Did not receive rate control agent in the ED within 12 hours, pregnant, incarcerated
- Intervention: Intravenous Diltiazem
- Comparison: Intravenous Metoprolol
- Outcome:
- Primary Outcome: Adverse events – hypotension (systolic BP<90 mmHg requiring fluid bolus or vasopressor administration), bradycardia (HR <60 bpm), worsening heart failure (increase in oxygen requirements by at least two liters within four hours or the need for inotrope within 48hrs)
- Secondary Outcomes: Incidence of rate control failure, admission level of care, ED length of stay, hospital length of stay, in-hospital mortality
- Type of Study: A single-center, retrospective study
Authors’ Conclusions: “There was no difference in total adverse effects between HFrEF patients treated with diltiazem vs metoprolol for acute AF. However, patients with diltiazem had higher incidence of worsening CHF symptoms defined as increased oxygen requirement within four hours or initiation of inotropic support within 48 h.”
 Quality Checklist for Observational Study:
Quality Checklist for Observational Study:
- Did the study address a clearly focused issue? Yes
- Did the authors use an appropriate method to answer their question? Yes
- Was the cohort recruited in an acceptable way? Unsure
- Was the exposure accurately measured to minimize bias? Unsure
- Was the outcome accurately measured to minimize bias? Unsure
- Have the authors identified all important confounding factors? Unsure
- Was the follow up of subjects complete enough? Yes
- How precise are the results? Unsure
- Do you believe the results? Yes
- Can the results be applied to the local population? Unsure
- Do the results of this study fit with other available evidence? Yes
- Funding of the Study? No conflicts of interest noted
Results: They screened 169 patients and included 125 (57 receiving diltiazem and 68 receiving metoprolol). The mean age was 62 years, 76% were male and the average ejection fracture was 16%. The mean initial dose was 16mg for diltiazem and 5mg for metoprolol.
Key Result: No statistical difference in adverse effects due to the interventions
- Primary Outcome: Composite outcome of adverse effects due to the interventions (32% vs 21%, P = 0.217)
- No statistical difference in any of the components of the composite outcome except for worsening CHF symptoms (33% vs. 15%, P = 0.019).
- Worsening CHF was driven by increased oxygen requirement within four hours
- Secondary Outcomes: No statistical difference in any of the secondary outcomes. Admission level of care was 33% vs 32% general, 51% vs 44% step-down and 16% vs 24% ICU.


The most obvious nerdy point limiting this study is the observational design. That means that unmeasured confounders cannot be controlled and could bias the results.
- Unbalanced Groups – Patients who received diltiazem were younger with higher baseline blood pressures (BP), so they may have been less likely to become hypotensive, which was defined primarily as systolic BP < 90 mmHg, rather than a measured drop in BP.
- Small Sample Size – There was an 11% absolute difference between the two drugs and incidence of adverse effects. This difference was not statistically significant. It is possible that a larger sample size would have reported a difference that was statistically significant. However, the observational nature of the study would only provide low-level evidence.
- Observer-Expectancy Effect – Discussion of the article mentions guidelines recommending against the use of diltiazem in patients with AF + RVR with HFrEF as it may worsen HF, despite minimal confirmatory evidence. Outcomes measured by increased oxygen requirement and inotrope administration can be subjective, and it is possible a greater number of patients in this cohort received interventions based on provider expectations.
- Lack of Comparator Group – It may have been useful to include a cohort of patients with AF + RVR without heart failure and examine whether their adverse effects would have been similar.
- Parametric and Non-parametric Data Analysis – Parametric data analysis is typically performed when data is normally distributed, and non-parametric data is best analyzed when data is not normally distributed. Common tests for parametric data analysis are the chi-square test, student t-test, ANOVA by sum of squares, among others; tests non-parametric data analysis are Fisher exact test, Wilcoxon signed rank test, Mann-whitney U test, ANOVA by rank, and Spearman rank coefficient. Prior studies have noted applying parametric statistical test to nonnormally distributed data reduces power and increases type II error. In this study, descriptive statistics were used for baseline data analysis which typically is used for nonnormally distributed data. Non-parametric tests may have affected the statistical significance of the data.
For more information on Parametric and Non-Parametric Data Analysis check out these links:
- Parametric and Nonparametric: Demystifying the Terms. By Tanya Hoskin, a statistician in the Mayo Clinic Department of Health Sciences.
- Choosing Between a Nonparametric Test and a Parametric Test. Minitab Blog Editor. 19 February, 2015.
- Parametric and Non-parametric tests for comparing two or more groups. UK Faculty of Public Health.
- Parametric versus nonparametric statistical tests: the length of stay example. Qualls et al. AEM 2010
Comment on Authors’ Conclusion Compared to SGEM Conclusion: We agree with the authors’ conclusions, although would make a friendly amendment to the first sentence to say: There was no STATISTICALLY SIGNIFICANT difference in total adverse effects between HFrEF patients treated with diltiazem vs metoprolol for acute AF.
SGEM Bottom Line: There is insufficient evidence to suggest a difference in total adverse outcomes for patients presenting to the ED in atrial fibrillation with rapid ventricular response treated with IV diltiazem vs metoprolol.
Case Resolution: The patient is given 5 mg of IV metoprolol as a push dose and his heart rate improves to the low 100s. He is feeling improved and thanks you for your help. The patient is subsequently admitted to the hospital for further workup and management.

Dr. Timlin Glaser
Clinical Application: It all depends. The evidence is weak to suggest one treatment over another and physicians will need to rely more upon their clinical judgment. It may be prudent to use a beta blocker in a patient who is already on a beta blocker at home. Although overall adverse events have been similar between beta blockers and CCB in the literature thus far, this study suggests Diltiazem may have a higher risk of worsening heart failure, while metoprolol may be more likely to cause hypotension. This is consistent with the current AHA guidelines for rate control in patients with atrial fibrillation and CHF.

Dr. Matt Murphy
What Do I Tell the Patient? Your heart is beating too fast, and we need to slow it down. One of the medications we use is like the medication you take at home. Another one works differently but can be used for the same purpose. Both may drop your blood pressure critically low or worsen your ability to breathe. If this happens, we can give you fluids or medication to raise your blood pressure or give you oxygen to help you breathe.
Keener Kontest: Dave Michaelson won again. He knew On June 15, 1667, the first direct blood transfusion to a human was performed by the physician Jean-Baptiste Denis, when he gave a feverish young man approximately 12 ounces of blood taken from a lamb.
Listen to the podcast to hear this weeks’ trivia question. If you know the answer, send an email to TheSGEM@gmail.com with “keener” in the subject line. The first correct answer will receive a cool skeptical prize.
Remember to be skeptical of anything you learn, even if you heard it on the Skeptics’ Guide to Emergency Medicine.
References:
January, C. T., Wann, L. S., Alpert, J. S., Calkins, H., Cigarroa, J. E., Cleveland Jr, J. C., … & Yancy, C. W. (2014). 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines and the Heart Rhythm Society. Circulation, 130(23), 2071-2104.







You must be logged in to post a comment.