Podcast: Play in new window
Subscribe: RSS
Date: September 28th, 2022
Reference: Hartford et al. Disparities in the emergency department management of pediatric migraine by race, ethnicity, and language preference. AEM September 2022.
Guest Skeptic: Dr. Lauren Westafer is an Assistant Professor in the Department of Emergency Medicine at the University of Massachusetts Medical School – Baystate. She is the cofounder of FOAMcast and is a pulmonary embolism and implementation science researcher.
Case: A 15-year-old patient presents to the Emergency Department with a unilateral pounding headache. The headache is similar to prior migraine headaches. They have photophobia but no vision changes, weakness, numbness, tingling, or neurologic deficits. They took 400 mg ibuprofen at home without relief. The patient and their mother ask what the next steps will be and what type of medication will be administered.
Background: We have looked at migraine treatment a few times on the SGEM. That includes an episode on steroids to prevent bounce back visits to the ED (SGEM#28), ketorolac for acute treatment (SGEM#66), acupuncture for prophylaxis (SGEM#211) and a calcitonin gene-related peptide antagonist (SGEM#279).
Patients with migraines often present to the ED looking for pain relief. There are many therapeutic options available to clinicians to address their pain. Unfortunately, poor pain control persists despite the Joint Commission on Accreditation of Healthcare Organizations (JCAHO) making pain “the fifth vital sign” in 2001 to raise the awareness of oligoanalgesia in the ED.
Despite the limitation of having a subjective measure as a vital sign, the problem of oligoanalgesia (poor pain management) persists (Motov and Khan). Some groups of patients who are at greater risk than others (elderly, women, mentally ill, certain ethnic groups, and insurance status).
Children represent one group that is less likely to receive adequate analgesia. (Brown et al, Selbst and Clark). It is not well documented, whether gaps in pain assessment and treatment exist in conditions in which opioids are not indicated, such as migraine headaches. It is hypothesized that race, ethnicity and language (REaL) could also be independently associated with pain control.
Clinical Question: Is there an association between patient demographics (race, ethnicity, and language) and pain management among pediatric ED patients presenting with migraine headaches?
Reference: Hartford et al. Disparities in the emergency department management of pediatric migraine by race, ethnicity, and language preference. AEM September 2022.
- Population: All patients treated in a single pediatric ED with at least one migraine-relevant medication using an ED migraine pathway from pathway inception (October 14, 2016) through February 28, 2020.
- Excluded: Repeat encounters
- Intervention: Intravenous (IV) medications +/- oral (PO)/intranasal (IN)
- Comparison: Oral or intranasal medications only
- Outcome:
- Primary Outcome: Treatment group assignment according to race, ethnicity and language (REaL) categories.
- Secondary Outcomes: Pain intensity scores using the age-appropriate scale (FACES or 0-10 pain scale), ED length of stay, ED charges (billing data)

Dr. Emily Hartford
This is an SGEMHOP episode which means we have the lead author on the show. Dr. Emily Hartford is as assistant professor in Pediatric Emergency Medicine at the University of Washington and Seattle Children’s Hospital. She works to improve equity for patients of diverse backgrounds in the ED as well as in global partnerships to improve pediatric emergency education.
This study was part of a quality improvement project that involved a migraine protocol (see below).

Authors’ Conclusions: “In this retrospective analysis of pediatric migraine patients in the ED, we found that race/ethnicity and language for care were significantly associated with odds of receiving intravenous therapies compared to oral or intranasal treatments.”
 Quality Checklist for Observational Study:
Quality Checklist for Observational Study:
- Did the study address a clearly focused issue? Yes
- Did the authors use an appropriate method to answer their question? Yes
- Was the cohort recruited in an acceptable way? Yes
- Was the exposure accurately measured to minimize bias? Yes
- Was the outcome accurately measured to minimize bias? Yes
- Have the authors identified all-important confounding? Unsure
- Was the follow up of subjects complete enough? Yes
- How precise are the results? Somewhat
- Do you believe the results? Yes
- Can the results be applied to the local population? Unsure
- Do the results of this study fit with other available evidence? Yes
- Conflicts of Interest? None
Results: They included 833 pediatric ED patients with migraine in the study. The median age was 14.8 years and two-thirds were female. There were 51% non-Hispanic White (nHW), 23% Hispanic, 8.3% Black or African American, 4.3% Asian. Of the 833 patients, 546 (65.5%) received intravenous (IV) medications.
Key Result: There were differences in the treatment of pain associations with race, ethnicity, and language in pediatric migraine patients.
- Primary Outcome: Treatment group assignment according to REaL categories.
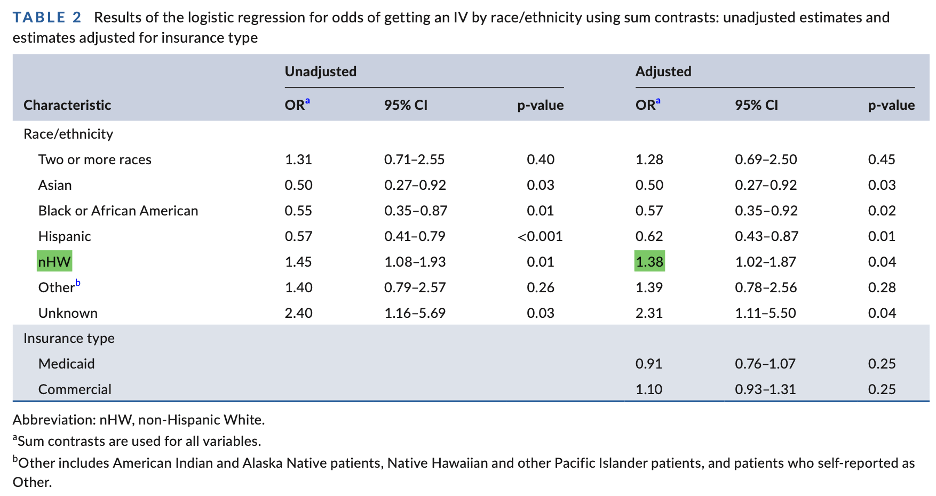 The adjusted odds of receiving IV medication by race/ethnicity was highest among those who identified as non-Hispanic White race with an adjusted odds ratio (aOR) of 1.38 (95% CI 1.02-1.87) and lower among those who self-identified as Asian, Black or African American, or Hispanic.
The adjusted odds of receiving IV medication by race/ethnicity was highest among those who identified as non-Hispanic White race with an adjusted odds ratio (aOR) of 1.38 (95% CI 1.02-1.87) and lower among those who self-identified as Asian, Black or African American, or Hispanic.

The aOR of receiving IV medication was 1.41 (95% CI 1.13 -1.77) in those who spoke English compared to 0.71 (95% CI 0.57-0.89) in those who spoke a language other than English.
- Secondary Outcomes: Pain intensity scores using the age-appropriate scale (FACES or 0-10 pain scale), ED length of stay, ED charges (billing data)
The change in pain intensity scores over time were similar between PO only treatment and IV treatment groups. However, there was somewhat greater improvement in the IV group.
Median LOS was 3.4 hours in the PO only group and 5.2 hours in the IV ± PO group. This gave a median difference of 1.8 hours (95% CI 1.6–2.0). However, there was not any statistically significant differences in this metric based upon race/ethnicity.
Median charges were $1,173 for the PO only group and significantly higher at $3,199 for the IV group. They assessed charges for the IV group only because PO/IN charges were likely based on static CPT values by billing coders and had no variability, and reported no statistical differences.

1. Sample Size in Racial Groups: In this study, the majority (51%) of the patients self-identified as non-Hispanic White, with < 5% identifying as Asian (4.2%), 2 or more races (4.6%), or Black/African-American (8.3%). How confident in these comparisons and associations should we be?
While the percentage of several REaL groups was indeed small, we did capture every individual patient that presented to our ED on the migraine pathway over the study timespan, so the results reflect what actually happened. Measurements of uncertainty, such as confidence intervals, reflect what might have happened under the same data-generating process as we experienced, and could reflect predictive/future patterns had we not subsequently started an intervention to address these disparities. While our results may or may not generalize to other institutions, they definitely reflect our own experiences, and as such we’re quite confident that the results suggest a need to improve.
2. Selection of Covariates: In your models, covariates included race/ethnicity groups, language type, and insurance type (public/private). Typically, in analyses, we adjust for covariates based on literature or theory. Why were only these included? Are there other important variables that you would have liked to include?
There’s a rough statistical rule of thumb that states you need a sample size of about 96 to usefully estimate the intercept (i.e. overall prevalence) in a logistic regression. So even with more than 800 patients in our study, we were still constrained by n size in including either additional variables or estimating interactions (the latter of which typically require an n size 4x higher than non-interaction analyses). You might expect that insurance type and race/ethnicity would have some statistical interactions in the United States, for example, but we did not have the n to estimate that. In addition, insurance type is a rough surrogate for SES in the absence of any other ways to measure SES status of patients; more direct measures of SES would have been nice to include, were they available.
3. Patient-Oriented Outcomes: Your outcomes included IV vs PO/IN, pain intensity, LOS, and charges. Did you collect data on patient preferences or satisfaction with treatment?
At the time of our analysis, we did not have access to patient satisfaction data than spanned our timeline, as our hospital had changed survey vendors and had not yet updated the data warehouse with those newer results. In addition, it could be difficult to compare results from two different vendors asking two different sets of patient satisfaction questions. It is an interesting question, however, and it would be nice to know more about that outcome.
4. Generalizability: This was conducted at a single freestanding academic pediatric hospital ED in the US. As a result, patient demographics may be different in other geographic locations and practices may vary at community EDs and those not affiliated with freestanding pediatric hospitals. In addition, REaL is not as “real” in other countries like UK, Europe, Canada, Australia, NZ,
Different countries have different ways of measuring and understanding variables such as race and ethnicity.
5. Collinearity: Language type and race/ethnicity were not included in the same regression models because they were strongly dependent. This is an example of collinearity, or a situation where two or more predictor variables are closely related to one another.
Comment on Authors’ Conclusion Compared to SGEM Conclusion: We agree with the authors’ conclusion.
SGEM Bottom Line: Non-Hispanic White English-speaking pediatric patients presenting to the ED are more likely to receive IV medication to treat their migraine headache compared to other races/ethnicities and non-English speaking patients.
Case Resolution: Listen to the podcast to hear how Emily would resolve the case.
Clinical Application: We should be aware that there can be some REaL (race, ethnicity and language) associations predicting which pediatric patients presenting to the ED will receive IV medication.
What Do I Tell the Patient? Listen to the podcast to hear Emily’s answer on how she talks to patients.
Keener Kontest: Last weeks’ winner was Ryker Kiel from Wyoming. They knew Chinese Hamster Ovary cells were used to produce Tenecteplase.
Listen to the podcast this week to hear the keener contest question. If you are the first person to email the correct answer to TheSGEM@gmail.com with “keener” in the subject line you will receive a cool skeptical prize.
SGEMHOP: Now it is your turn SGEMers. What do you think of these REaL issues in the ED with pediatric pain management? What questions do you have Emily? Tweet your comments using #SGEMHOP or post your feedback on the SGEM blog. The best social media feedback will be published in AEM.

Remember to be skeptical of anything you learn, even if you heard it on the Skeptics’ Guide to Emergency Medicine.







You must be logged in to post a comment.