Podcast: Play in new window
Subscribe: RSS
Date: August 19th, 2021
Reference: Pantell et al. Evaluation and management of well-appearing febrile infants 8 to 60 days old. Pediatrics 2021
Guest Skeptic: Dr. Dennis Ren is a pediatric emergency medicine fellow at Children’s National Hospital in Washington, DC.
Case: A 25-day-old, full-term boy presents to the emergency department with fever. His parents report that he felt warm that evening, and they found that he had a rectal temperature of 38.2°C (100.8°F). He has an older sister at home with a cough and rhinorrhea. Overall, he has no symptoms and appears well. He has continued to feed normally and produce wet diapers. The parents ask you, “Do you really think he needs any additional testing? He probably caught something from his sister, right?”
 Background: Parents often bring their infants to the ED with concerns about fever. They can develop a real “fever fear” or “feverphobia” and often need reassurance that fever alone is not dangerous. We have talked about pediatric fever and fever fear with Dr. Anthony Crocco from Sketchy EBM back on SGEM#95 and made a “Ranthony” video on the topic. The American Academy of Pediatrics says that
Background: Parents often bring their infants to the ED with concerns about fever. They can develop a real “fever fear” or “feverphobia” and often need reassurance that fever alone is not dangerous. We have talked about pediatric fever and fever fear with Dr. Anthony Crocco from Sketchy EBM back on SGEM#95 and made a “Ranthony” video on the topic. The American Academy of Pediatrics says that
“…fever, in and of itself, is not known to endanger a generally healthy child. In contrast, fever may actually be of benefit; thus, the real goal of antipyretic therapy is not simply to normalize body temperature but to improve the overall comfort and well-being of the child.”
However, fever without source in infants less than three months of age represents a significant diagnostic dilemma for clinicians. Several clinical decision instruments had been developed previously, including the Rochester (Jaskiewicz et al 1994), Boston (Baskin et al 1992) and Philadelphia (Baker et al 1993) criteria to help clinicians stratify the risk of significant bacterial infections. A new clinical decision instrument called the Step-by-Step approach was reviewed on SGEM#171.
SGEM#171 Bottom Line: If you have availability of serum procalcitonin measurement in a clinically relevant time frame, the Step-by-Step approach to fever without source in infants 90 days old or younger is better than using the Rochester criteria or Lab-score methods. With the caveat that you should be careful with infants between 22-28 days old or those who present within two hours of fever onset.
We have been trying to optimize our approach to evaluating and managing febrile infants for more than four decades. Our goal is to identify the febrile infants with urinary tract infection, bacteremia, and bacterial meningitis (or what was referred to as serious bacterial infections) while simultaneously trying to spare them from invasive and potentially unnecessary procedures like lumbar punctures or the possible iatrogenic consequences of empiric antibiotics or hospitalization.
Several risk stratification tools have been published over the years. These clinical decision instruments included subjective clinical criteria along with pre-determined thresholds for lab criteria like white blood cell count (WBC) and immature to total neutrophil ratio. Unfortunately, these criteria may not be appropriate in the current era. In fact, the Modified Boston and Philadelphia Criteria for invasive bacterial infections may misclassify almost one-third of infants with bacterial meningitis.
With routine screening of pregnant women, improvements in food safety, and conjugate pneumococcal vaccines, we have seen a decrease in Group B streptococcus, Listeria, and Streptococcus pneumoniae infections in infants. Instead, there has been a shift to Gram-negative organisms being the most common culprits in bacterial infections in infants.
Simultaneously, our ability to test for infection has advanced with the use of inflammatory markers (IM) like procalcitonin and C-reactive protein (CRP) as well as polymerase chain reaction (PCR) testing for rapid identification of multiple viruses and bacteria.
Clinical Question: What are recommendations for evaluating and managing well-appearing, term infants, 8 to 60 days of age with fever ≥38°C?
Reference: Pantell et al. Evaluation and management of well-appearing febrile infants 8 to 60 days old. Pediatrics 2021
Authors’ Conclusion: “Three algorithms summarize the recommendations for infants 8 to 21 days of age, 22 to 28 days of age, and 29 to 60 days of age. The recommendations in this guideline do not indicate an exclusive course of treatment or serve as a standard of medical care. Variations, taking into account individual circumstances, may be appropriate.”
 Quality Checklist for A Guideline:
Quality Checklist for A Guideline:
- The study population included or focused on those in the emergency department? No
- An explicit and sensible process was used to identify, select and combine evidence? Yes
- The quality of the evidence was explicitly assessed using a validated instrument? Yes
- An explicit and sensible process was used to the relative value of different outcomes? Yes
- The guideline thoughtfully balances desirable and undesirable effects? Yes
- The guideline accounts for important recent developments Yes/Unsure
- The guidelines has been peer-reviewed and tested? Yes/No
- Practical, actionable, and clinically important recommendations are made? Yes
- The guideline authors’ conflicts of interest are fully reported, transparent and unlikely to sway the recommendations of the guidelines? Yes
Key Recommendations:

There are four key components to considered in evaluating the well-appearing febrile infant and three algorithms based on the age of the infant.
- Four Key Components of Evaluation:
- Urine
- Blood culture
- Inflammatory Markers (IM)
- Procalcitonin >0.5 ng/mL
- Absolute neutrophil count (ANC) > 4,000 mm3 or >5,200 mm3 (There are two ANC cutoffs included based on the PECARN study and Febrile Young Infant Research Collaborativestudy)
- CRP >20 mg/L
- Temperature > 38.5°C
- Cerebrospinal Fluid (CSF) from lumbar puncture (LP)
- Algorithms At a Glance: There are three age groups (8-21d, 22-28d and 29-60d). All age groups get urine and blood cultures. Inflammatory markers are considered optional for the youngest group. The youngest group gets an LP, antibiotics and admitted while the older two groups may get an LP and antibiotics and may be discharged home.

Infants 8 to 21 Days of Age
This is a straightforward group and not a big change from previous practice. We should still be conservative with this group. These infants are all getting a full work up including urine, blood, and CSF. They are being treated with empiric antibiotics and staying in the hospital.

Dr. Archie Cochrane
The inflammatory markers are optional (Grade B, Weak Recommendation) as they do not really change decision to administer antimicrobials or disposition. This follows Archie Cochrane’s approach to testing:
- “Before ordering a test, decide what you will do if it is (1) positive or (2) negative. If both answers are the same, don’t take the test”.
We should be also cautious regarding herpes simplex virus (HSV) infection in this age group and may also consider adding acyclovir coverage in addition to empiric antibiotics.


Infants 22 to 28 Days of Age
This is where there is some nuance and room for shared decision making. We are still going to obtain urine and blood. This is where the inflammatory markers can be used to guide further management.
If any IM is abnormal, these guidelines recommend performing an LP and obtaining CSF (Grade C, Moderate Recommendation). However, even if all IMs are normal, the clinician can still choose to perform a LP.
If the decision is made to defer LP, these patients will need to stay in the hospital. The choice of administering empiric antimicrobials in a situation where an LP is not performed is dependent on a discussion of the potential harms and potential benefits between clinician and family. While the risk of meningitis is lower in this age group, empiric treatment without CSF may result in partially treated meningitis.
A key thing to remember for this algorithm and age group is that we should not send these patients home without obtaining an interpretable CSF. If the urine studies are normal, IM are normal, CSF is normal or enterovirus positive, these patients can be discharged home after receiving a dose of parenteral antibiotics (Grade C, Moderate Recommendation) with proper anticipatory guidance and return precautions and follow up in 24 hours.

Infants 29 to 60 Days of Age
This algorithm has the potential to really decrease the number of LPs and allow us to send more infants home based on the IMs. We are still going to start by obtaining urine, blood culture, and IMs.
Circumcised boys may be exempted from urine studies given their risk of urinary tract infection is <1%. In the setting of having normal IMs, LP may be deferred (Grade B, Moderate Recommendation) even with a positive urinalysis. Patients with positive urinalysis and normal IMs can be discharged home on oral antibiotics with close follow up in 12 to 24 hours.
 If urinalysis is negative and the IMs are normal, these patients may be sent home without a lumbar puncture and without antimicrobial therapy. They should be closely observed, provided with strict return precautions, and have follow up arranged within 24 to 36 hours.
If urinalysis is negative and the IMs are normal, these patients may be sent home without a lumbar puncture and without antimicrobial therapy. They should be closely observed, provided with strict return precautions, and have follow up arranged within 24 to 36 hours.
If the IMs are elevated, things get a bit tricky. The guidelines state that a LP may be performed (Grade C, Weak Recommendation). This is different from the previous age group where the recommendation was that LP should be performed in the setting of abnormal IMs.
If CSF is negative with positive or negative urinalysis, you may give them a dose of antimicrobial and still send them home. If CSF is not obtained or uninterpretable, you should give a dose of IV antimicrobial and observe in the hospital or discharge home. This requires a very careful discussion with the family about the potential harms, potential benefits, return precautions, and follow up.

 1. Age Groups: These guidelines are another step in the effort for lowering the age threshold for performing a full sepsis work up (blood, urine, CSF). We have come a long way from performing full work ups in infants up to 90 days to lowering that threshold now to 21 days. Important to note that infants less than eight days were not included in this guideline.
1. Age Groups: These guidelines are another step in the effort for lowering the age threshold for performing a full sepsis work up (blood, urine, CSF). We have come a long way from performing full work ups in infants up to 90 days to lowering that threshold now to 21 days. Important to note that infants less than eight days were not included in this guideline.
What a difference a week makes. For the 22 to 28 day-old group, it is still reasonable to err on the side of being more conservative. Again, we want to emphasize that if no CSF is obtained, these patients cannot go home. For the 29 to 60 day-old group, these guidelines offer a lot more room for discussion and shared decision making about LP, antibiotics, and disposition.
Keep in mind that the overall trend is that risk of bacteremia and bacterial meningitis tend to decline with age, but the cut offs are still arbitrary. Obviously, there is not a dichotomy between infants and risk between 28 and 29 days of age or even 60 and 61 days of age. Risk is on a spectrum and will also require clinical judgment.
 2. Stop Saying Serious Bacterial Infection (SBI): Many studies use the term SBI, but the authors recommend that we stop using this term and be specific as to what we are describing. Urinary tract infections are much more common than bacteremia and bacterial meningitis so putting all of these in one category can affect accuracy of prediction models. Additionally, bacterial meningitis is rare so finding a large enough sample for accurate prediction is very difficult.
2. Stop Saying Serious Bacterial Infection (SBI): Many studies use the term SBI, but the authors recommend that we stop using this term and be specific as to what we are describing. Urinary tract infections are much more common than bacteremia and bacterial meningitis so putting all of these in one category can affect accuracy of prediction models. Additionally, bacterial meningitis is rare so finding a large enough sample for accurate prediction is very difficult.
3. Inflammatory Markers: Stop using white blood count (WBC). There are multiple inflammatory markers proposed in these guidelines. The authors emphasize that no individual IM is reliable for risk stratification. We rarely use one piece of laboratory information to make a clinical decision. Medical decisions take place in a clinical context. Most of the IMs are laboratory values but it is important to note the one that is not, temperature >38.5°C. Of the laboratory criteria, the authors favor using procalcitonin with either ANC or CRP. If procalcitonin is not available or the results do not return in a reasonable time, they recommend both ANC and CRP and temperature >38.5°C. They provide values for area under the curve for procalcitonin, CRP, and ANC. Additionally, they recommend against using WBC for risk stratification.
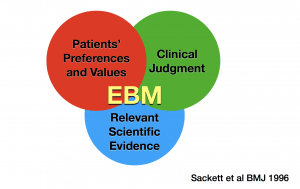 4. Evidence-Based Medicine (Parental and Clinician Input): This clinical guideline really hits the mark with its consideration of all three pillars of EBM. It incorporates and acknowledges clinical judgement, scientific evidence, and the patient or family’s values and preferences in its recommendations. It is emphasized that many of these decisions should be made through collaborative discussion between families and clinicians acting in the best interest of the patient.
4. Evidence-Based Medicine (Parental and Clinician Input): This clinical guideline really hits the mark with its consideration of all three pillars of EBM. It incorporates and acknowledges clinical judgement, scientific evidence, and the patient or family’s values and preferences in its recommendations. It is emphasized that many of these decisions should be made through collaborative discussion between families and clinicians acting in the best interest of the patient.
5. Future Directions: Where do we go from here? These new AAP guidelines with three algorithms are like a clinical decision instrument to help clinicians risk stratify patients. There are three steps in the development and testing of clinical decision instruments. The first step has been completed with the creation and publication of these AAP algorithms.
The next step will be to test and prospectively validate what combination of inflammatory markers will yield the most accurate prediction model for a specific infection in different clinical environments.
The third and final step, which is often not done, is to assess the impact of these algorithms on the clinical practice in these well-appearing febrile infants. It will also be interesting to see what role viral testing, biomarkers, and genomic testing will play.
Comment on Authors’ Conclusion Compared to SGEM Conclusion: We generally agree with the authors’ conclusion.
SGEM Bottom Line: The algorithms in this AAP clinical practice guideline have the potential to decrease the number of lumbar punctures, hospitalizations, and antibiotic treatment in well-appearing, febrile infants. Keep in mind that these are guidelines and do not replace clinician judgement. They also do not claim to be the “standard of care”. It is important to consider the risk tolerance and aversion of the clinician and family when implementing these recommendations.
Case Resolution: You explain to the parents your concerns and performing some urine and blood testing to help me determine the next best steps. After some time passes, the urinalysis does not appear to demonstrate any signs of urinary tract infection. The procalcitonin level is <0.5 ng/mL. The ANC is <4,000 mm3. You discuss the option of a lumbar puncture with the parents who express that they really do not want that their baby to undergo that procedure. After further discussion, they agree to admission in the hospital without antibiotics for observation.

Dr. Dennis Ren
Clinical Application: These new AAP guidelines offer an evidence-based approach for evaluating and managing the well-appearing, febrile infant. It has three algorithms based on age and 21 key action statements with discussion of potential harms and potential benefits. It may or may not decrease the lumbar punctures, hospital stays, and empiric antibiotics in the older age groups and emphasizes partnering with the family in making these decisions.
What Do I Tell the Patient (Parents)? Your baby’s young age makes me worried for the possibility of a serious infection. The blood and urine testing we performed are reassuring so far. We can discuss the option of performing a lumbar puncture to evaluate for infection in the cerebrospinal fluid. It may help us decide about whether it would be safe to go home. However, I understand your hesitation so let’s have you stay overnight in the hospital for observation.
Keener Kontest: Last weeks’ winner was Angela T. She knew the first successful IO blood transfusion was done via the sternum.
Listen to the podcast this week to hear the trivia question. Email your answer to TheSGEM@gmail.com with “keener” in the subject line. The first correct answer will receive a cool skeptical prize.
Remember to be skeptical of anything you learn, even if you heard it on the Skeptics’ Guide to Emergency Medicine.








You must be logged in to post a comment.