Podcast: Play in new window
Subscribe: RSS
[display_podcast]
Date: August 26th, 2014
Guest Skeptic: Dr. Chris Bond. Chris is a clinical lecturer and emergency physician at the University of Calgary, #FOAM blogger, dogma basher, wine and food supergeek. Chris has a blog called SOCMOB, is part of the REBEL-EM Alliance and did a blog entry on colchicine for pericarditis.
Reference: Imazio, et al. A Randomized Trial of Colchicine for Acute Pericarditis. NEJM 2013
Case Scenario: A 33 year-old woman presents to emergency department with sharp retrosternal chest pain which is pleuritic in nature. Well’s low and PERC negative. ECG consistent with acute pericarditis. Other lab investigations normal.
Question: Is colchicine more effective in combination than standard anti-inflammatory therapy for acute pericarditis, than standard anti-inflammatory therapy alone?
Background: Pericarditis is inflammation of the pericardium, most often from an infectious or idiopathic cause. There are also other less common etiologies like neoplastic, autoimmune, drugs, trauma and radiation.
The classic history is positional, pleuritic chest pain radiating to the trapezius muscles. The pain is worsened by lying flat and relieved sitting forward. Other historical clues would be concurrent or recent infectious symptoms, eg. low grade fever, cough, general weakness.
On exam there are two important diagnostic findings: a pericardial friction rub, and a pericardial effusion on bedside U/S.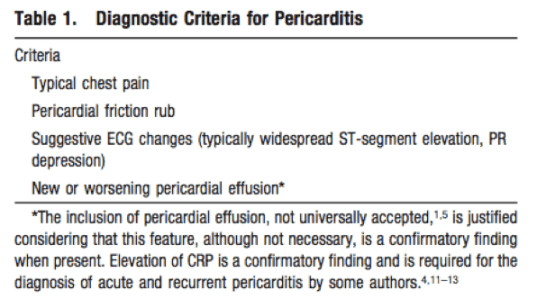
For investigations, the ECG is the diagnostic test of choice, which should show widespread ST elevation, and PR depression inferiorly and PR elevation in aVR. However, this is a very simplified description of the pericarditis ECG, and I would highly recommend listeners check out Amal Mattu’s pericarditis EKG videos.
For blood tests, the WBC and CRP are insensitive and non-specific. The troponin is used to look for myocardial involvement (myopericarditis), however, with the new high-sensitivity troponins, we may be calling myopericarditis more in the future.
To summarize, there are generally four consensus diagnostic criteria:
- Classic Chest Pain
- Friction Rub
- Effusion on Ultrasound
- ECG Changes
Colchicine is a plant derived alkaloid that functions as a microtubule inhibitor. It comes from the autumn crocus or meadow saffron plant. It is one of the oldest anti-inflammatories and has been used to treat rheumatic diseases for about 2500 years. Traditional uses include treatment of familial Mediterranean fever, Behcet’s disease and gout.
Unfortunately, colchicine also has a pretty narrow therapeutic window, so you can imagine that there was quite a bit of colchicine toxicity back in the day.
For some good information as background material check out Controversial Issues in the Management of Pericardial Disease. Imazio et al Circulation 2010;121:916-928
Reference: Imazio, et al. A Randomized Trial of Colchicine for Acute Pericarditis. NEJM 2013
- Population: 240 adult patients were enrolled from from five general hospitals in Northern Italy. All were diagnosed with a first episode of acute pericarditis. This was defined as at least two of the following; typical chest pain (pleuritic, improved sitting up and forward), pericardial friction rub, ST elevation or PR depression, new or worsening pericardial effusion.
- Exclusions: TB, neoplastic, or purulent pericarditis; severe liver disease or current aminotransferase levels >1.5x upper limit of normal; serum creatinine >2.5 mg/dL; skeletal myopathy or serum creatinine kinase level above the upper limit of the normal range; blood dyscrasia; inflammatory bowel disease; hypersensitivity to colchicines or other contraindication to its use; current treatment with colchicines; life expectancy of 18 months or less; pregnant or lactating women. Also patients with evidence of myopericarditis, as indicated by an elevation in the serum troponin level.
- Intervention: Colchicine (0.5 – 1.0 mg) daily for 3 months in conjunction with conventional anti-inflammatories.
- Comparison:
- ASA 800 mg or ibuprofen 600 mg every 8 hours for 7 to 10 days, followed by a taper for 4 weeks.
- Prednisone (0.2-0.5 mg/kg) daily was given to patients with contraindications to aspirin therapy (allergy, peptic ulcer disease, anticoagulant use i.e patient’s with high risk of bleeding).
- All patients in both groups received gastroduodenal prophylaxis with proton-pump inhibitors.
- Outcome:
- Primary Outcome: Incessant or recurrent pericarditis. Recurrent pericarditis was defined by symptom-free interval of 6 weeks or longer after the initial episode of pericarditis. Recurrence was documented by recurrent pain and one or more of the following signs: pericardial friction rub; ECG changes; pericardial effusion on echocardiography; or elevation in WBC or ESR or C-reactive protein.
- Secondary Outcome: Symptom persistence at 72 hours, remission within 1 week, number of recurrences, the time to first recurrence, disease-related hospitalization, cardiac tamponade, and constrictive pericarditis.
Authors’ Conclusions: “The use of colchicine in addition to standard anti-inflammatory therapy with GI prophylaxis in the treatment of acute pericarditis reduced the rate of refractory or recurrent episodes and increased the time to recurrence when compared to placebo.”
 Quality Check List for Random Control Trials:
Quality Check List for Random Control Trials:
- The study population included or focused on those in the ED? Unsure
- The patients were adequately randomized? Yes
- The randomization process was concealed? Yes
- The patients were analyzed in the groups to which they were randomized? Yes
- The study patients were recruited consecutively (i.e. no selection bias)? Yes
- The patients in both groups were similar with respect to prognostic factors. Yes
- All participants (patients, clinicians, outcome assessors) were unaware of group allocation. Yes
- All groups were treated equally except for the intervention. Yes
- Follow-up was complete (i.e. at least 80% for both groups). Yes
- All patient-important outcomes were considered. Yes
- The treatment effect was large enough and precise enough to be clinically significant. Yes
 Key Results: Based upon the data presented the NNT for the primary outcome to prevent the one case of recurrent or incessant pericarditis was 4.8
Key Results: Based upon the data presented the NNT for the primary outcome to prevent the one case of recurrent or incessant pericarditis was 4.8
(95% CI 3-11). Figure2 in the manuscript showed the Kaplan-Meier Survival Curves for freedom from incessant or recurrent pericarditis.
Kaplan-Meier survival curve is the probability of surviving in a given length of time while considering small time intervals. It is a standard way of expressing the number of subjects living for a certain amount of time after treatment from clinical trials.

- Secondary Outcomes:
- Symptom persistance 72hrs (ARR 20.8%, NNT=5)
- Recurrence frequency (ARR 31%, NNT=3)
- Hospitalizations (ARR 9.2%, NNT=11)
- Remission 1 week (ARR 26.7%, NNT=4)
- Prolonged time to first recurrence (24.7 weeks vs. 17.7 weeks)

This was a well done RCT with excellent adherence to drug regimens (95%) and no losses to follow-up. The effects of colchicine was seen early and the benefits were sustained out to 18 months. Benefits were seen both in the primary and secondary outcomes.
The authors reported a NNT of 4 but recomputed the NNT is 4.8 with 95% CI 3-11, so actual applied NNT is 5.
This paper was funded by the pharmaceutical industry, as disclosed via a non-influence statement in the article.
As with many RCT the study was powered to show benefit but underpowered to detect rare adverse effects.
The main side effects in both groups were gastrointestinal (GI) disturbances, and were statistically insignificant between groups (9.2% in the colchicine group, compared to 8.3% in the placebo group, P=0.67). It is possible the side effects were caused by the standard therapies (ASA, ibuprofen, corticosteroids) all despite prophylactic GI protection with proton pump inhibitor.
SGEM Bottom Line: Adding colchicine to usual anti-inflammatory management with GI prophylaxis prevents recurrence or refractory pericarditis symptoms with a NNT of 5. The most common side effect being diarrhea. Strict exclusion criteria limits application to uncomplicated pericarditis without systemic manifestations or evidence of elevated cardiac biomarkers (including non-specific troponitis).
Case Resolution: This 33 year-old woman diagnosed with pericarditis was given a prescription for ibuprofen 600mg TID for 7 days followed by a tapering dose over 1 month, colchicine 0.5mg daily for three months and proton pump inhibitor for 3 months. She was also referred to cardiology for on-going follow-up.
Clinical Application: Colchicine (0.5-1.0mg) daily for three months in conjunction with conventional anti-inflammatories and GI prophylaxis can be used for acute non-suppurative pericarditis to prevent recurrence or refractory symptoms.

Dr. Chris Bond
What Do I Tell Patients: You have inflammation around your heart called pericarditis. Anti-infammatory drugs like ibuprofen and ASA can help treat your symptoms. An additional medicine called colchicine has been shown to prevent prolonged symptoms. Colchicine has also been shown to prevent pericarditis from happening again. These two type of medications can be hard on the stomach so we are going to give you something to protect your gut. The most common side effect to these effective pericarditis treatments is diarrhea.
Keener Kontest: Marcus Prescott knew that Sussman and Fitch published the first study on thrombolysis in stroke in 1958. Thrombolysis with fibrinolysin in cerebral arterial occlusion. JAMA. 1958 Aug 2;167(14):1705–1709.
Listen to the podcast to hear this weeks keener question. If you know the answer send an email to TheSGEM@gmail.com with “keener” in the subject line. The first person to correctly answer the question will receive a cool skeptical prize.
Upcoming conferences:
Remember to be skeptical of anything you learn, even if you heard it on the Skeptics’ Guide to Emergency Medicine.








You must be logged in to post a comment.