Podcast: Play in new window
Subscribe: RSS
[display_podcast]
Date: May 20, 2013
Title: TNT (To Not Treat) with Prophylactic Antibiotics for Basilar Skull Fractures
 Case Scenario: An otherwise healthy 21yo male patient who has been drinking alcohol all day at the beach. He tries to jump into the back of his friends moving Jeep and does a face plant. He arrives by ambulance GSC 15 collar and boarded with racoon eyes. Because your small hospital does not have a CT scanner you ship him out for the CT head which shows a non-displaced basilar skull fracture. You admit him to hospital for neurological observation while the alcohol wears off. You wonder should you start prophylactic antibiotics to prevent meningitis?
Case Scenario: An otherwise healthy 21yo male patient who has been drinking alcohol all day at the beach. He tries to jump into the back of his friends moving Jeep and does a face plant. He arrives by ambulance GSC 15 collar and boarded with racoon eyes. Because your small hospital does not have a CT scanner you ship him out for the CT head which shows a non-displaced basilar skull fracture. You admit him to hospital for neurological observation while the alcohol wears off. You wonder should you start prophylactic antibiotics to prevent meningitis?
Question: Are prophylactic antibiotics effective in preventing meningitis in patients with basilar skull fractures?
Background: Basilar skull fractures from non-penetrating head trauma is estimated to by about 10%. Cerebral spinal fluid leakage associated basilar skull fractures is also about 10% with a range from 2-20%. The concern with basilar skull fracture is the direct contact of bacteria in the paranasal sinuses, nasopharynx or middle ear could predispose patients to meningitis. Physicians often give prophylactic antibiotics to decrease the risk of meningitis in these cases.
Signs/Symptoms of a Basilar Skull Fracture:
-
 Battle Sign
Battle Sign- Hearing loss
- Tympanic membrane perforation
- CSF otorrhea/rhinorrhea
- Bilateral periorbital eccymosis (Racoon eyes)
- Peripheral facial nerve palsy
- Vestibular dysfunction
- Anosmia
Reference: Ratilal BO, Costa J, Sampaio C, Pappamikail L. Antibiotic prophylaxis for preventing meningitis in patients with basilar skull fractures. Cochrane Database of Systematic Reviews 2011, Issue 8. Art. No.: CD004884.
- Population: Patients of any age with recent basilar skull fracture. 5 RCT’s (N=208) and 17 non RCTs (N=2168) analyzed separately.
- Intervention: Prophylactic antibiotics administered at the time of primary treatment of basilar skull fracture. n=109
- Control: Placebo n=99
- Outcome: Primary: Menigitis suspected clinically and confirmed by lumbar puncture. Secondary: All-cause mortality/meningitis-related mortality. Need for surgical correction in patients with CSF leakage. Non-CNS infection.
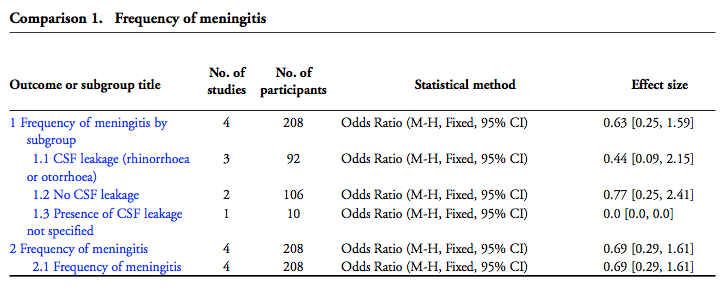
Results: 5 RCTs (n=208) and 17 non-RCTs (n=2168) All 208 participants from the 5 RCTs included in the meta-analysis. There were no significant differences between the two groups (antibiotic prophylaxis vs. and control). This included the primary outcome of meningitis and all the secondary outcomes (all-cause mortality, meningitis-related mortality, and need for surgical correction in patients with CSF leakage). A meta-analysis of the non-RCT had results similar to the RCT data. No adverse effects were reported with the use of antibiotic.
Authors Conclusions: “Currently available evidence from RCTs does not support prophylactic antibiotic use in patients with BSF, whether there is evidence of CSF leakage or not. Until more research is completed, the effectiveness of antibiotics in patients with BSF cannot be determined because studies published to date are flawed by biases. Large, appropriately designed RCTs are needed.”
BEEM Comments: The studies included in this review all had important methodological flaws. Curiously, the frequency of meningitis in the Eftekhar 2004 trial was significantly higher than in the other trials. This may be because they only enrolled patients with a basilar skull fracture and pneumocephalus. This could represent patients at higher risk for developing meningitis. There was no difference overall in the frequency of meningitis in the prophylactic antibiotic group versus the control group, even when the subgroups with and without CSF leakage were analyzed. There was a possible adverse effect of increasing susceptibility to infection with more pathogenic organisms in those treated with antibiotics. None of the studies reported data on outcomes of safety and tolerability of prophylactic antibiotics.
BEEM Bottom Line: There is no support for routine prophylactic antibiotics in all patients with basilar skull fracture. Further RCTs are needed to assess its benefits and risks clearly.
Case Resolution: You decide not to give prophylactic antibiotics to this young man who tried to jump into a moving vehicle and sustained a basilar skull fracture.
KEENER KONTEST: Last week’s winner was Chris Bond from Saskatoon and responsible for SOCMOB blog. He is TheSGEMs first repeat winner. Chris suggested Doxycycline 100 mg po BID as a nice choice for community acquired pneumonia in a 66yo woman on a calcium channel blocker as recommended by IDSA guidelines (Grade III rec) as alternative to Macrolide.
Be sure to listen to this weeks podcast for another chance to a cool skeptical prize. Email your answer to TheSGEM@gmail.com. Use “Keener Kontest” in the subject line. First one to email me the correct answer wins.
Dr. Anthony Crocco and I will be presenting the Best of BEEM at this years CAEP meeting in Vancouver next month. Please come by and say hello. If you are not attending this year than follow on Twitter @TheSGEM and Facebook.
Remember to be skeptical of anything you learn, even if you heard it on The Skeptics Guide to Emergency Medicine. Be safe this holiday long weekend. Talk with you next week.







You must be logged in to post a comment.